-
摘要
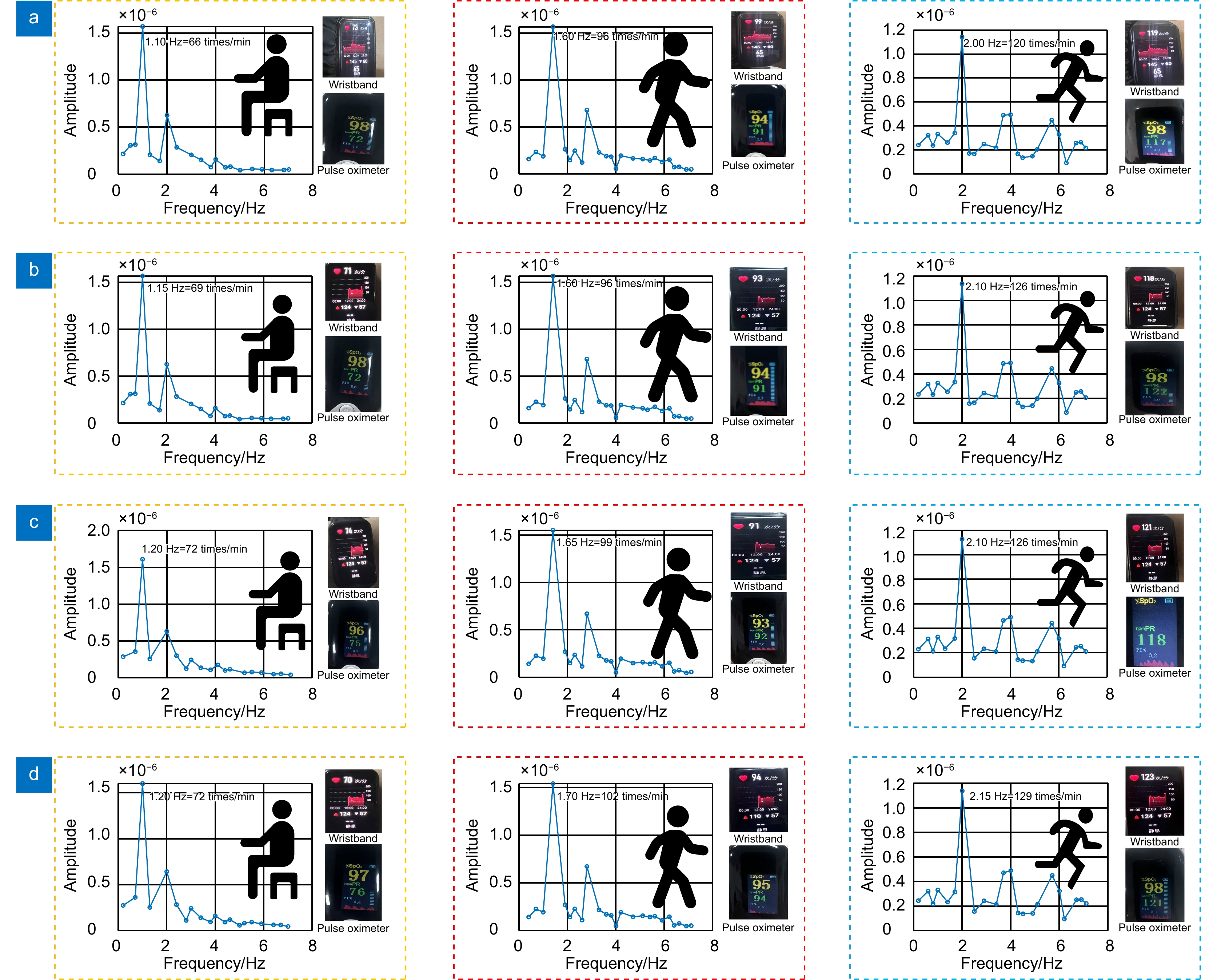
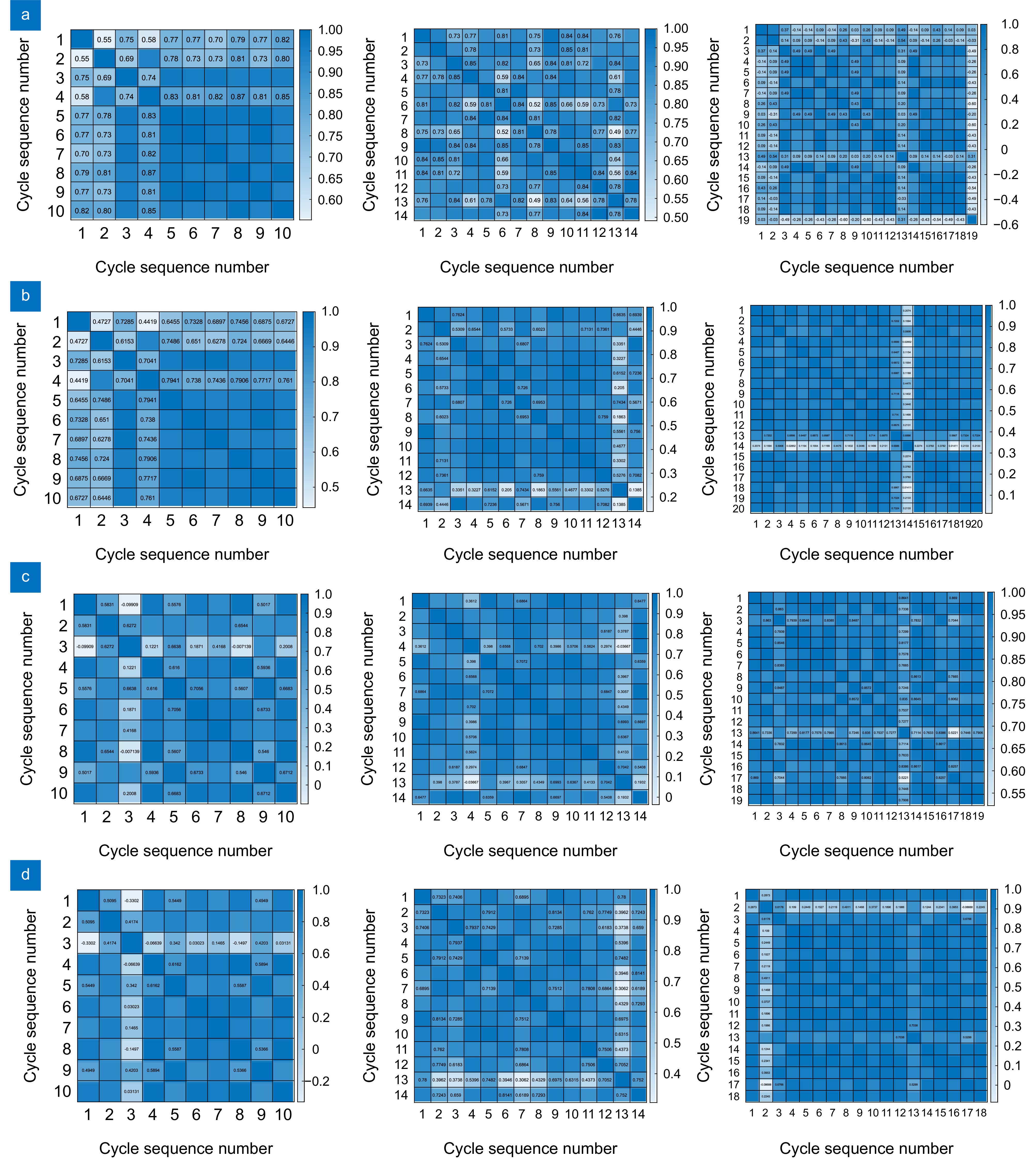
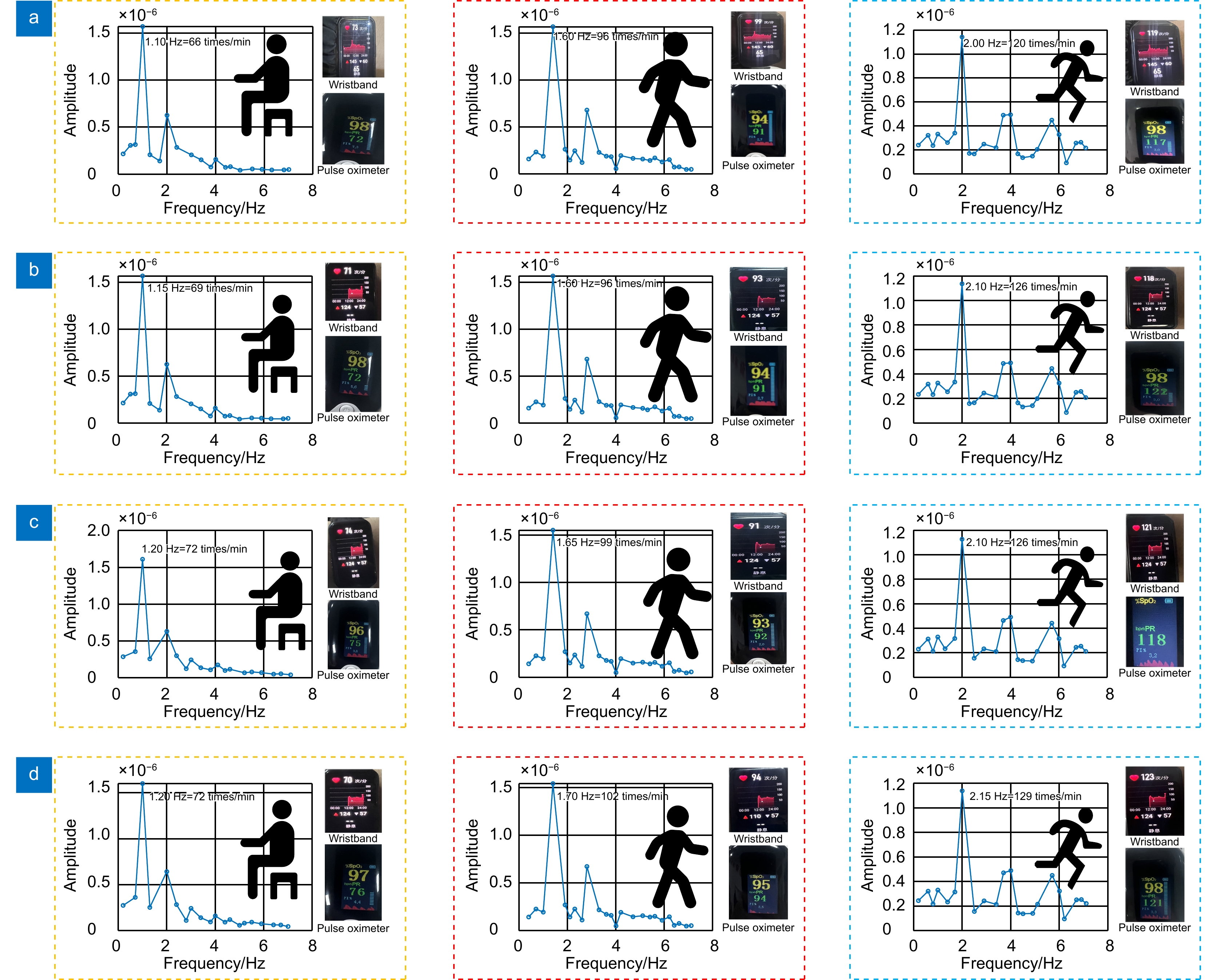
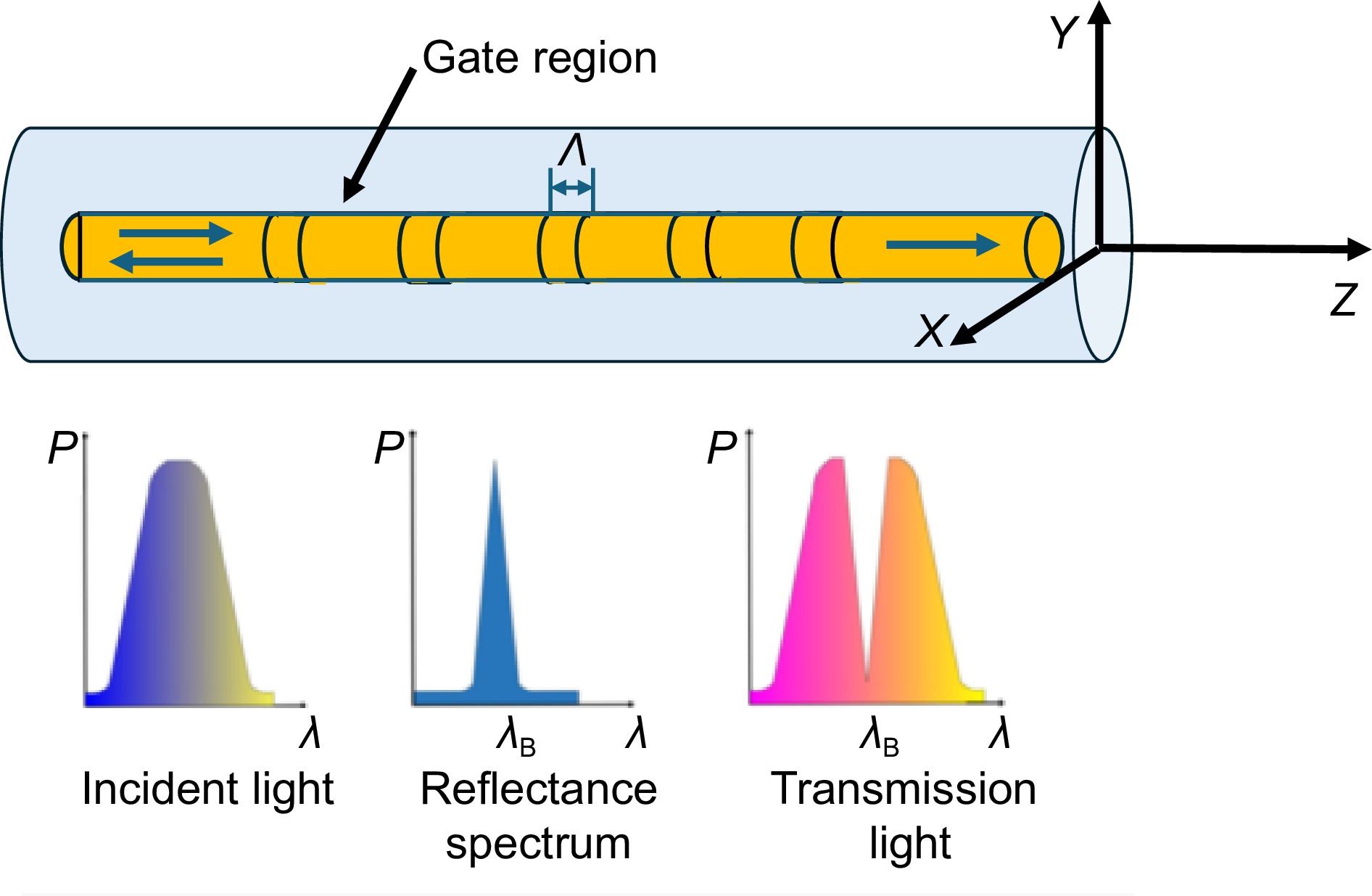
针对目前颈部脉搏监测装置不便携带、信号处理复杂等缺点,设计一款光纤布拉格光栅(fiber Bragg grating, FBG)颈部脉搏监测装置。使用该装置监测志愿者1、2在静坐和仰卧时3种状态(静息、运动和剧烈运动)下的颈部脉搏各10 s。利用傅里叶变换对其进行处理,得到其频率与手环、血氧仪监测的频率误差都小于10%,对不同状态的各自周期进行皮尔逊相关性分析,得到其相关性大于0.9。利用随机森林对其进行预测分析,得到其预测分析效果较好。分析结果表明,该颈部脉搏监测装置能够有效地监测人体颈部脉搏。
Abstract
In response to the current limitations of neck pulse monitoring devices, such as being inconvenient to carry and having complex signal processing, a fiber Bragg grating (FBG) based neck pulse monitoring device was designed. The device monitored two volunteers in three states (resting, exercise, and vigorous exercise) while sitting and lying down for 10 s each. Fourier transform was applied to process the data, and the frequency error between the neck pulse device, the wristband, and the pulse oximeter was found to be less than 10%. Pearson correlation analysis was conducted on the periods of different states, with the correlation coefficient exceeding 0.9. Random forest was used for predictive analysis, and the results showed good prediction performance. The analysis indicates that the neck pulse monitoring device is capable of effectively monitoring the pulse in the neck region of the human body.
-
Overview
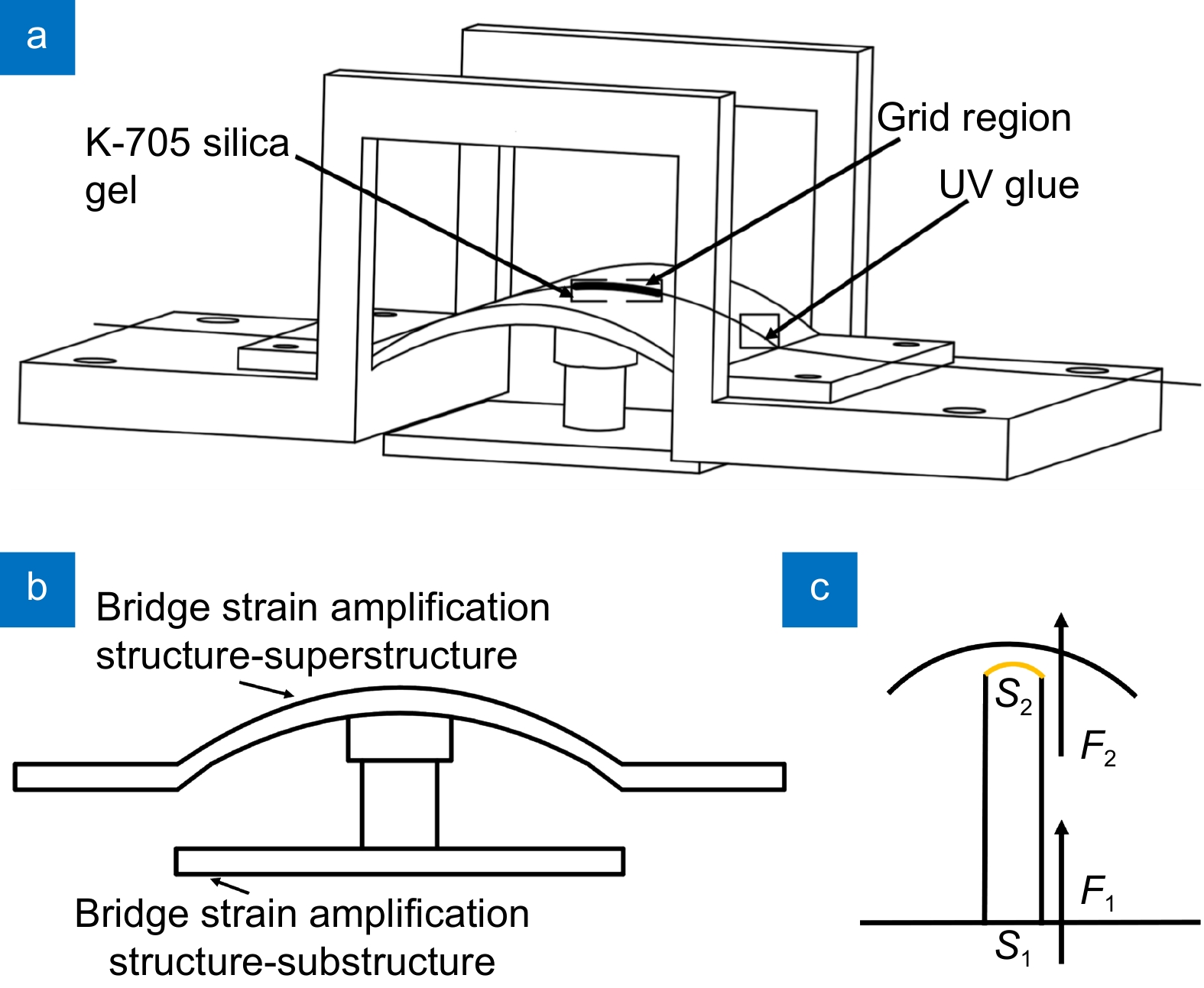
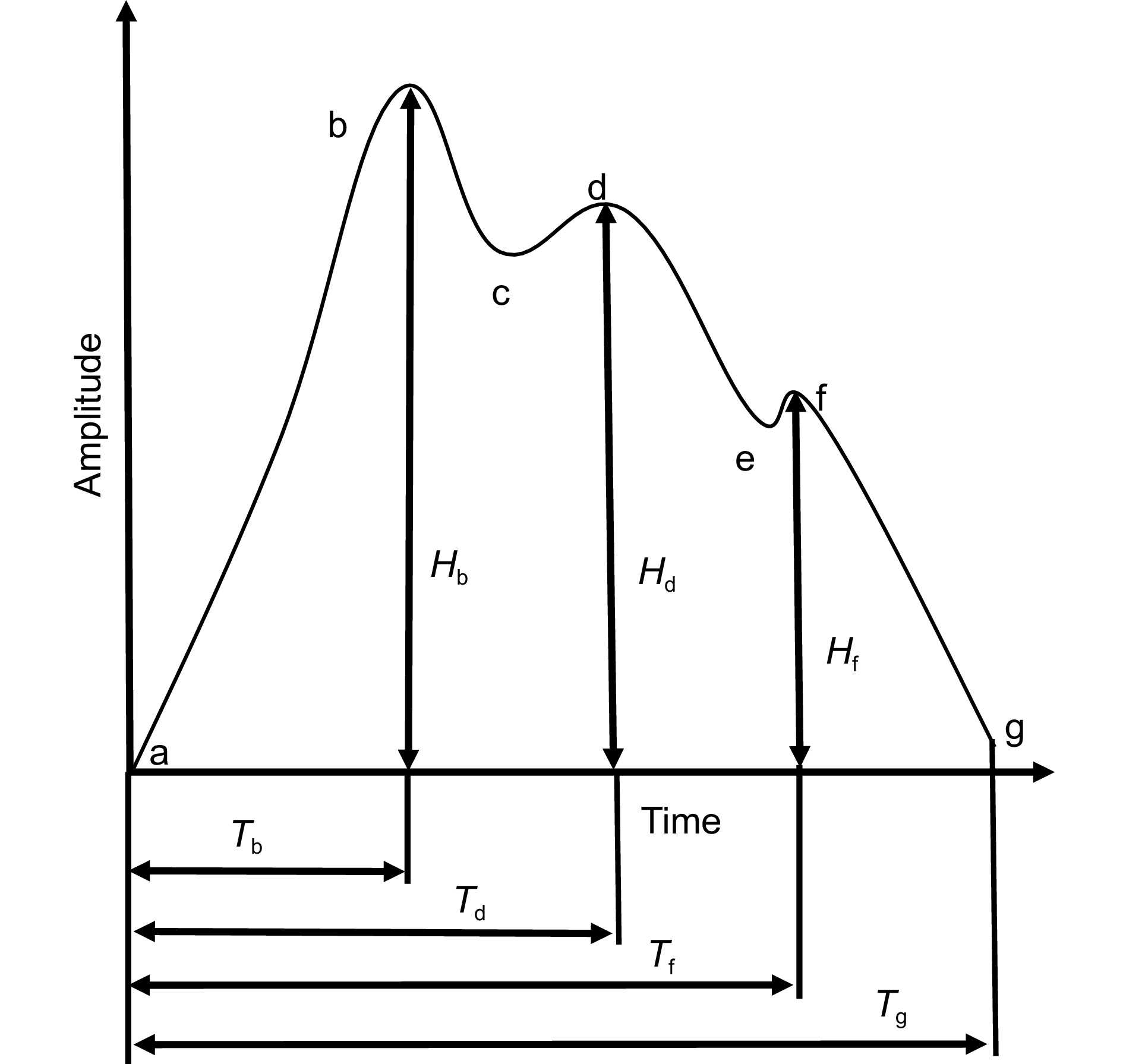
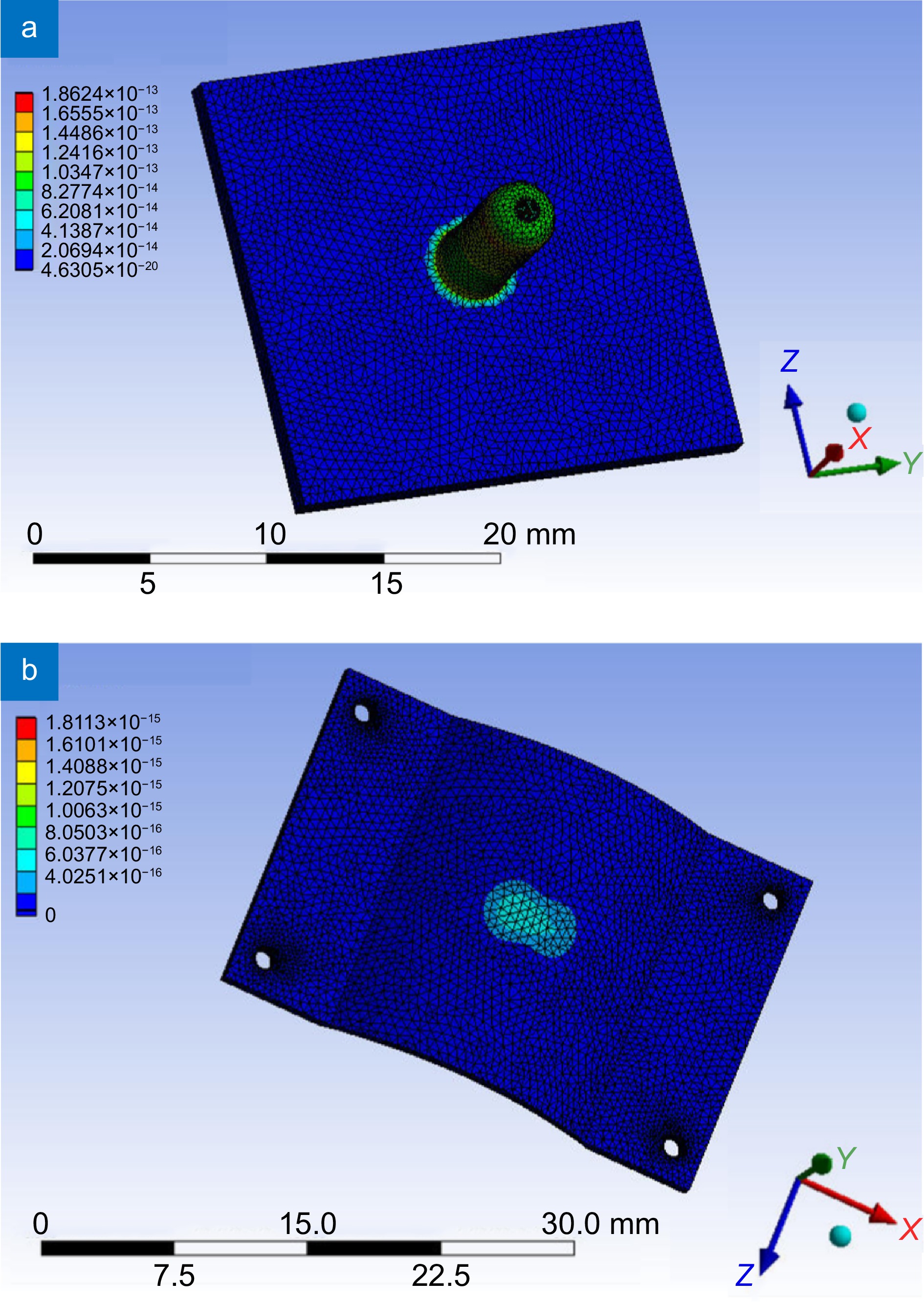
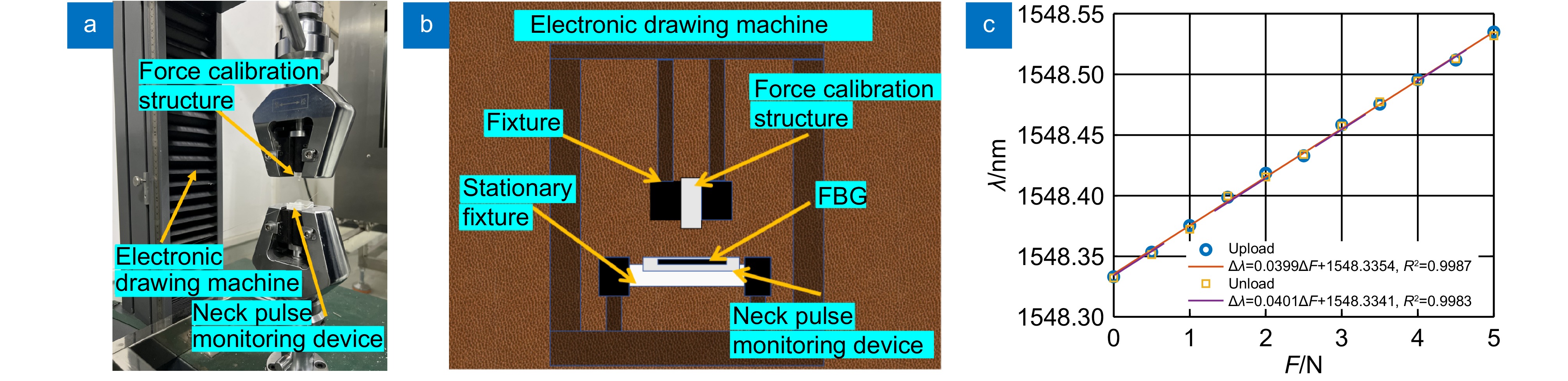
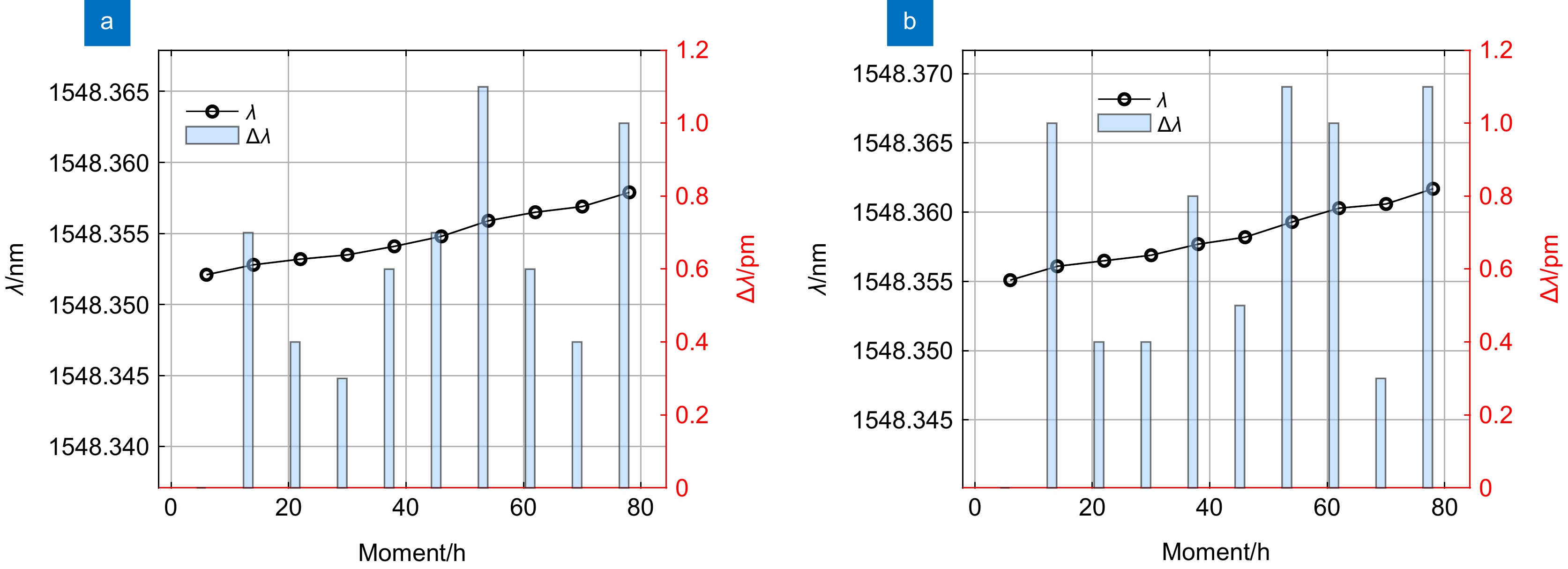
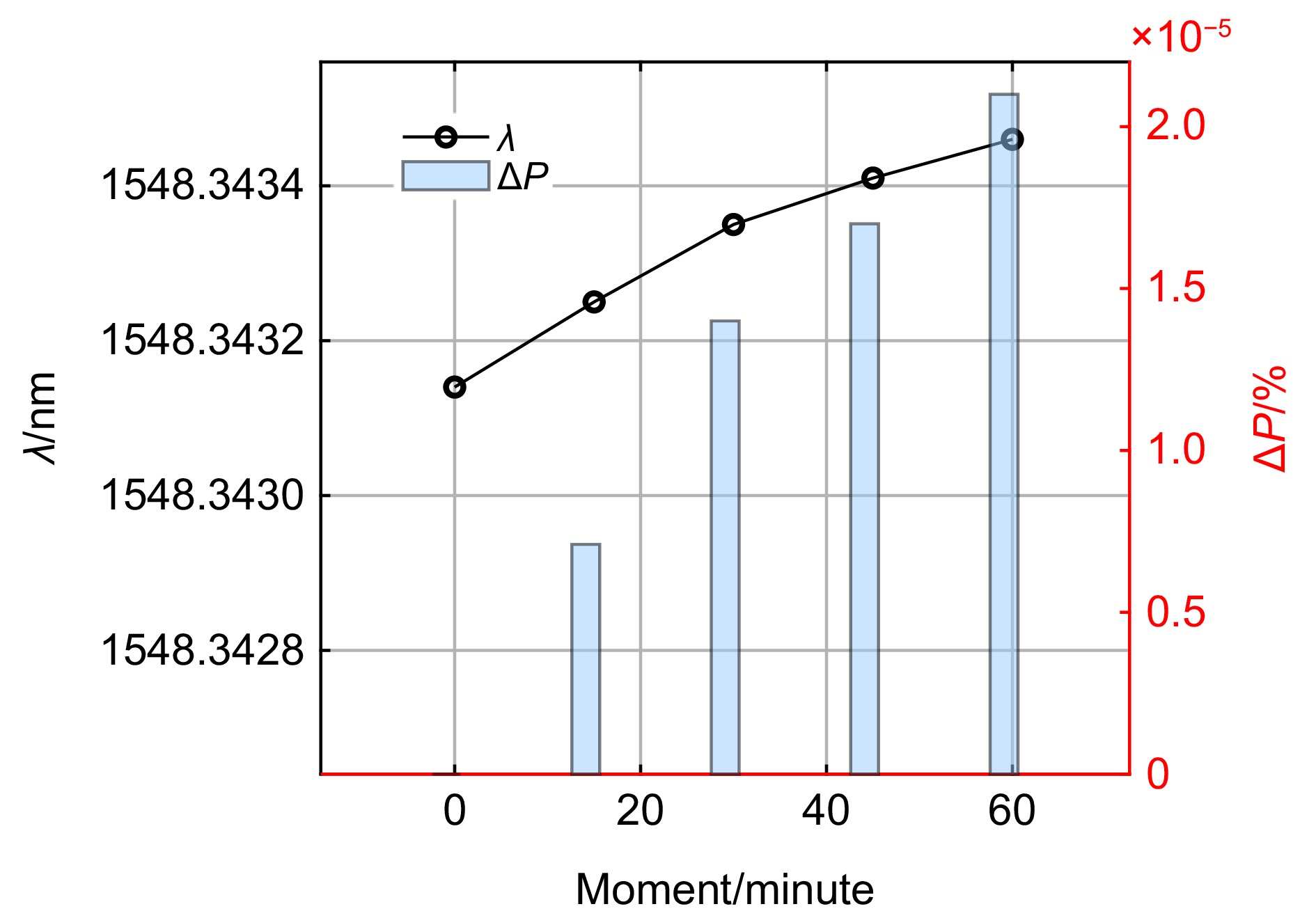
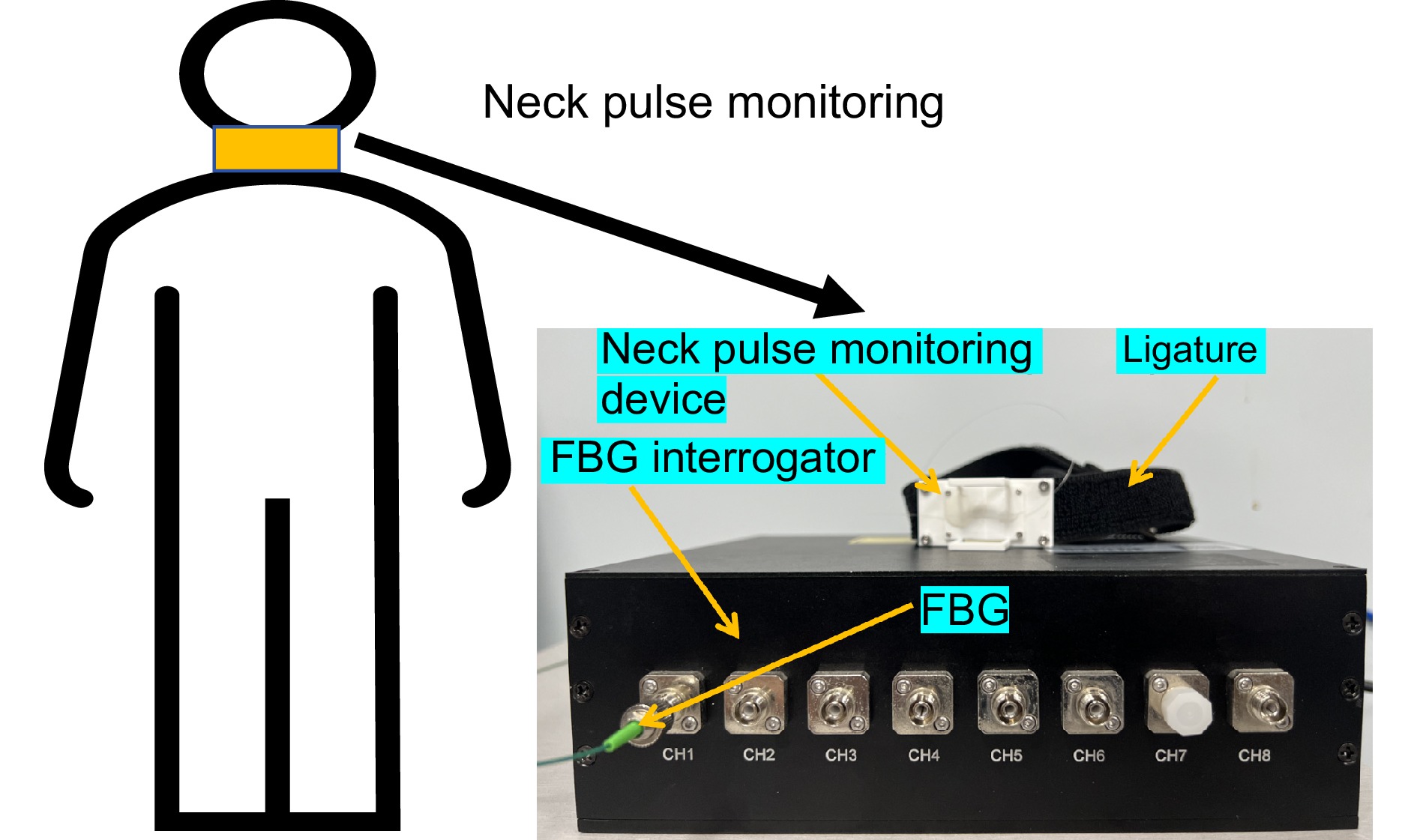
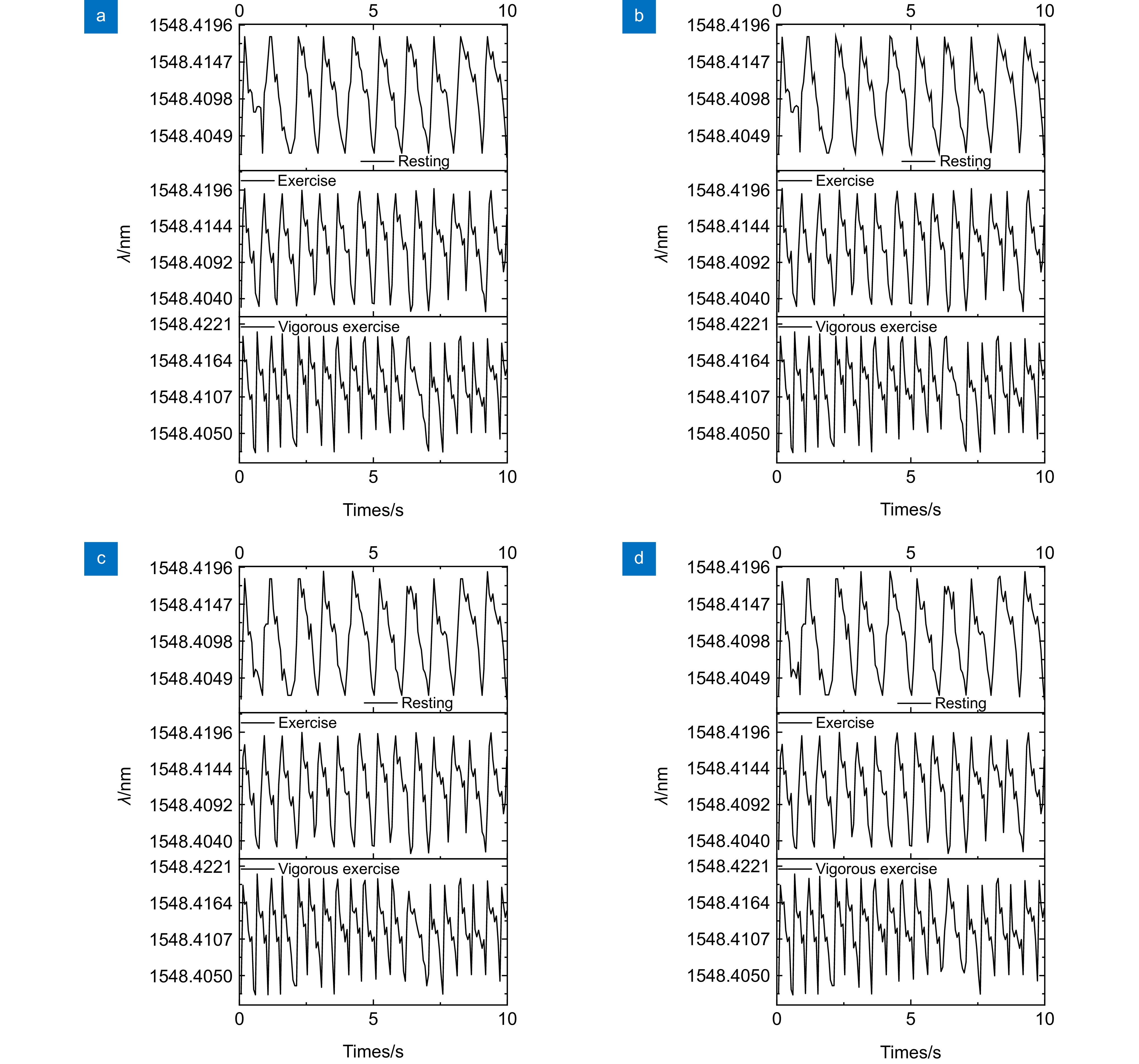
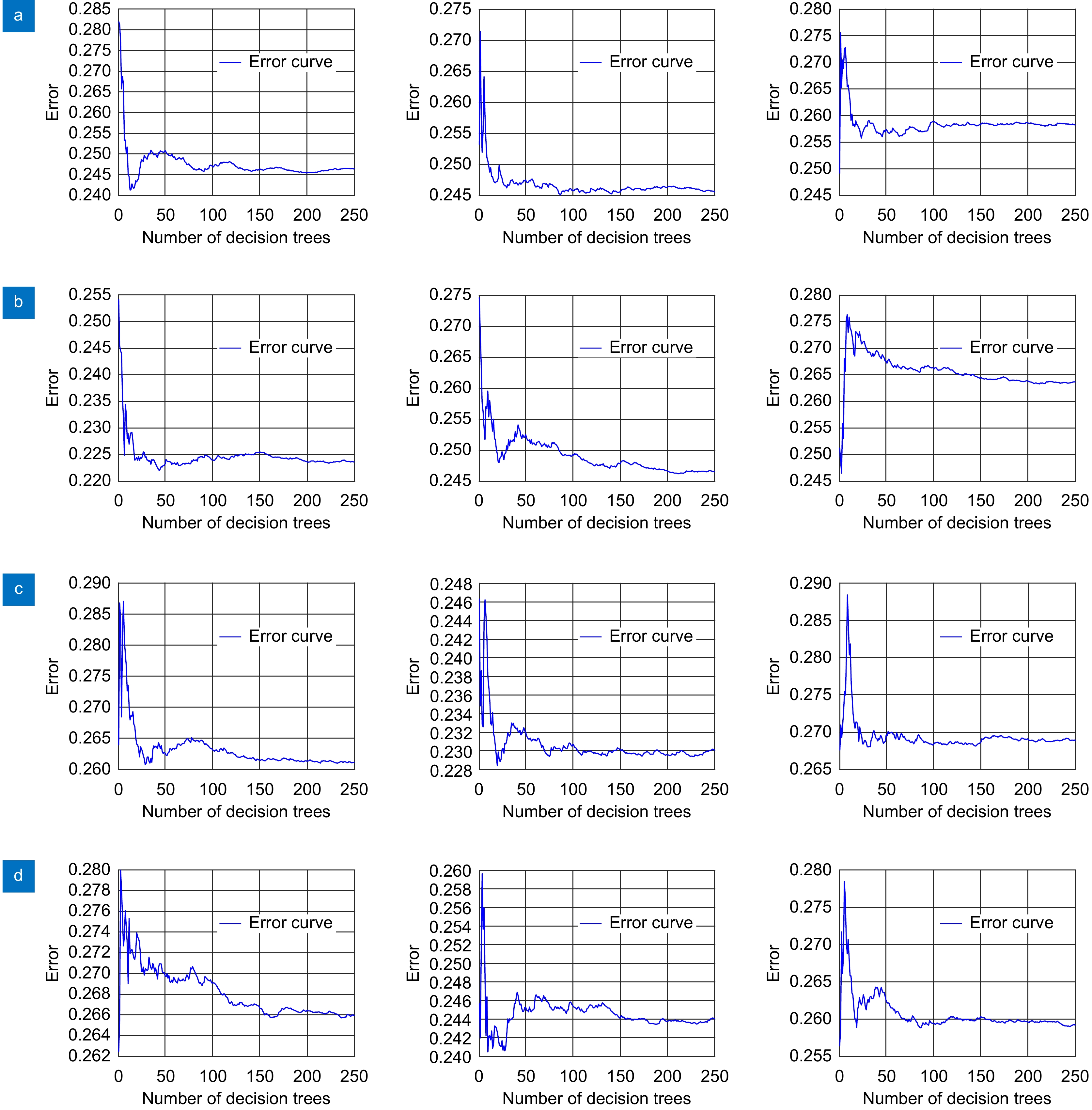
Overview: A wearable fiber Bragg grating neck pulse monitoring device has been designed to address the shortcomings of current neck pulse monitoring devices, including inconvenience in wearing and complex signal processing. This device is not affected by temperature, offers portability and comfort, enhances monitoring sensitivity, and can track the neck pulse frequency of the human body under different states. The device has been optimized for comfort, ensuring that users experience greater comfort during monitoring. Calibration experiments have shown that its pressure sensitivity is 40 pm/N, with a fitting goodness of 0.9985. The error between the theoretical sensitivity and the calibration experimental sensitivity is only 2.663%, which is relatively low. A temperature comparison experiment was conducted, and the maximum error was found to be 1.750%, demonstrating that the performance of the device is minimally affected within a certain temperature range. The device underwent 72 h aging experiments under temperature and force conditions, and the maximum wavelength variation at adjacent time points was 1.12 pm and 1.11 pm, indicating minimal change and proving that its performance is not significantly affected under these conditions. The device was subjected to a 1 h signal attenuation experiment, where the maximum attenuation rate was less than 0.1%, indicating that the signal attenuation over the hour was negligible. volunteer 1 used the device to monitor the neck pulse for 10 s at 15:00, 17:00, 19:00, 21:00, and 23:00 on the same day. The ICC coefficient of the five monitoring data points was 0.99383, indicating high consistency between the five sets of data. The device was used to monitor volunteers 1 and 2 under sitting and lying down in different states (resting, exercise, and vigorous exercise) for 10 s each, and it was observed that while the peaks and valleys of the pulse waves exhibited some differences, their periodicity was almost consistent. The first complete cycle of each state was processed and analyzed by spline interpolation, and the results of comparison with theoretical pulse wavelength changes showed consistent trends. Fourier transform processing was applied to the data, and the frequency error with that of wristbands and pulse oximeters was found to be less than 10%. Pearson correlation coefficient of the periods for different states yielded a correlation greater than 0.9. Finally, random forest was used for predictive analysis, and the evaluation results showed that the prediction was accurate. The analysis above indicates that the neck pulse monitoring device can effectively monitor the neck pulse of the human body.
-

-
图 14 静息、运动、剧烈运动状态的随机森林误差与决策树数目分析。 (a)志愿者1静坐;(b) 志愿者1仰卧;(c) 志愿者2静坐;(d)志愿者2仰卧
Figure 14. Random forest error and decision tree number analysis of resting, exercise and vigorous exercise states. (a) Volunteer 1 sit;(b) Volunteer 1 lies in supine position; (c) Volunteer 2 sit; (d) Volunteer 2 lies in supine position
表 1 监测装置-手环-血氧仪脉搏监测对比数据
Table 1. Monitoring device-bracelet - oximeter pulse monitoring comparison data
Volunteer Posture State Frequency/(times/min) Ws/% Wx/% Monitoring device Wristband Oximeter Volunteer 1 Sit Resting 66 73 72 9.58 6.69 Exercise 96 99 91 3.03 5.50 Vigorous exercise 120 119 117 0.83 2.56 Supine Resting 69 71 72 2.82 4.17 Exercise 96 93 91 3.23 5.50 Vigorous exercise 126 118 122 6.78 3.28 Volunteer 2 Sit Resting 72 74 75 2.70 4.00 Exercise 99 91 92 8.79 7.61 Vigorous exercise 126 121 118 4.13 6.78 Supine Resting 72 70 76 2.86 5.26 Exercise 102 94 94 8.51 8.51 Vigorous exercise 129 123 121 4.88 6.61 表 2 静息、运动、剧烈运动状态的评价指标
Table 2. Evaluation indicators of resting, exercise, and vigorous exercise states
Posture Dataset Index Resting Exercise Vigorous exercise Volume 1 sit Training set MAE 0.4669 0.4631 0.4900 MBE -0.0021 0.0004 0.0033 RMSE 0.4589 0.4325 0.4711 Prediction set MAE 0.4671 0.4694 0.4993 MBE 0.0012 0.0009 0.0026 RMSE 0.4626 0.4256 0.4692 Volume 1 lies in supine position Training set MAE 0.4787 0.4497 0.4735 MBE −0.0015 0.0041 0.0002 RMSE 0.4871 0.4806 0.4838 Prediction set MAE 0.4878 0.4478 0.4809 MBE −0.0022 −0.0011 −0.0013 RMSE 0.4817 0.4803 0.4823 Volume 2 sit Training set MAE 0.4866 0.4742 0.4844 MBE −0.0031 −0.0016 −0.0033 RMSE 0.4789 0.4854 0.4857 Prediction set MAE 0.4927 0.4616 0.4856 MBE 0.0011 −0.0348 0.0015 RMSE 0.4819 0.4777 0.4801 Volume 2 lies in supine position Training set MAE 0.4712 0.4847 0.4685 MBE 0.0038 −0.0016 0.0012 RMSE 0.4815 0.4876 0.4883 Prediction set MAE 0.4739 0.4804 0.4692 MBE 0.0012 0.0011 −0.0019 RMSE 0.4905 0.4916 0.4811 -
参考文献
[1] Butlin M, Tan I, Qasem A, et al. Comparison of effects of peripheral vasculature on tonometric radial pulse and cuff-based brachial pulse waveform as used in estimation of central aortic pressures[C]//Proceedings of 2023 45th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), 2023: 1–4. https://doi.org/10.1109/EMBC40787.2023.10340973.
[2] Xue S K, Xu Z H, Wang Y X, et al. Simultaneous multi-person vital signs monitoring using multiple-input multiple-output FMCW millimeter wave radar[J]. AEU-Int J Electron Commun, 2025, 188: 155578. doi: 10.1016/j.aeue.2024.155578
[3] Gharamohammadi A, Bagheri M O, Abu-Sardanah S, et al. Smart furniture using radar technology for cardiac health monitoring[J]. Sci Rep, 2025, 15(1): 1392. doi: 10.1038/s41598-024-80062-5
[4] Seifizarei S, Elnaggar I, Anzanpour A, et al. Continuous radar-based heart rate monitoring using autocorrelation-based algorithm in intensive care unit[J]. IEEE J Biomed Health Inf, 2025, 1−9. doi: 10.1109/JBHI.2025.3527566
[5] Wang X, Li J J, Meng K Y, et al. Differential-deformation structured pressure sensor for stable measurement of superficial temporal artery pulse[J]. Nano Energy, 2025, 135: 110678. doi: 10.1016/j.nanoen.2025.110678
[6] Zhou J, Qu M J, Liu W T, et al. Continuous monitoring of blood pressure by measuring local pulse wave velocity using wearable micromachined ultrasonic probes[J]. IEEE Trans Biomed Eng, 2025, 1−10. doi: 10.1109/TBME.2024.3514878
[7] Jia H L, Gao Y Y, Zhou J K, et al. A deep learning-assisted skin-integrated pulse sensing system for reliable pulse monitoring and cardiac function assessment[J]. Nano Energy, 2024, 127: 109796. doi: 10.1016/J.NANOEN.2024.109796
[8] Khan A, Rashid M, Grabher G, et al. Autonomous triboelectric smart textile sensor for vital sign monitoring[J]. ACS Appl Mater Interfaces, 2024, 16(24): 31807−31816. doi: 10.1021/acsami.4c04689
[9] Yao J J, Qu C M, Chen Z H, et al. High-sensitive wearable capacitive pressure sensor with hemispherical porous electrode[J]. ACS Appl Electron Mater, 2024, 6(4): 2649−2658. doi: 10.1021/acsaelm.4c00210
[10] Shi C Y, Tang Z X, Zhang H, et al. Development of an FBG-based wearable sensor for simultaneous respiration and heartbeat measurement[J]. IEEE Trans Instrum Meas, 2023, 72: 4000409. doi: 10.1109/TIM.2022.3228276
[11] Li T L, Pei Q F, Zhao C. Plastic optical fiber sensor-based smart mattress for sleeping posture remote monitoring[C]//Proceedings of 2022 18th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob), 2022: 136–141. https://doi.org/10.1109/WiMob55322.2022.9941526.
[12] Leal-Junior A, Avellar L, Blanc W, et al. Opto-electronic smart home: heterogeneous optical sensors approaches and artificial intelligence for novel paradigms in remote monitoring[J]. IEEE Internet Things J, 2024, 11(6): 9587−9598. doi: 10.1109/JIOT.2023.3323481
[13] Guo Y, Tong X X, Shen Y X, et al. Wearable optical fiber beat frequency digital sensing system for real-time non-invasive multiple human physiological parameters monitoring[J]. J Lightwave Technol, 2023, 41(9): 2911−2920. doi: 10.1109/JLT.2023.3238476
[14] Shi C Y, Zhang H, Ni X L, et al. An FBG-based sensor with both wearable and handheld forms for carotid arterial pulse waveform measurement[J]. IEEE Trans Instrum Meas, 2023, 72: 7506610. doi: 10.1109/TIM.2023.3311052
[15] 张治胜. 基于光纤光栅的生理信号监测及分类算法研究[D]. 南昌: 南昌航空大学, 2023: 1–108. https://doi.org/10.27233/d.cnki.gnchc.2023.000763.
Zhang Z S. Research on physiological signal monitoring and classification algorithm based on fiber Bragg grating[D]. Nanchang: Nanchang Hangkong University, 2023: 1–108. https://doi.org/10.27233/d.cnki.gnchc.2023.000763.
[16] 邵涛平. 基于光纤柔性感知的人体生理参数实时监测系统[D]. 长春: 长春理工大学, 2024: 1–75. https://doi.org/10.26977/d.cnki.gccgc.2024.000325.
Shao T P. Real-time monitoring system for humanphysiological parameters based on optical fiberflexible sensing[D]. Changchun: Changchun University of Science and Technology, 2024: 1–75. https://doi.org/10.26977/d.cnki.gccgc.2024.000325.
[17] 陈勇, 姚知民, 刘焕淋, 等. 基于改进互补集成经验模态分解的脉搏波去噪[J]. 光学学报, 2024, 44(7): 0707001. doi: 10.3788/AOS231695
Chen Y, Yao Z M, Liu H L, et al. Pulse wave denoising based on improved complementary ensemble empirical mode decomposition[J]. Acta Optica Sin, 2024, 44(7): 0707001. doi: 10.3788/AOS231695
[18] Li Z Y, Tang X Z, Zhao T, et al. Highly sensitive skin-like wearable optical sensor for human physiological signals monitoring[J]. Opt Fiber Technol, 2024, 82: 103652. doi: 10.1016/j.yofte.2023.103652
[19] Kuang R F, Wang Z, Ma L, et al. Smart photonic wristband for pulse wave monitoring[J]. Opto-Electron Sci, 2024, 3(12): 240009. doi: 10.29026/oes.2024.240009
[20] Xie T T, Chen H, Xu Z W, et al. High precision strain sensing system based on optoelectronic oscillator for human pulse monitoring[J]. IEEE Sensors J, 2025, 25(4): 6355−6362. doi: 10.1109/JSEN.2024.3522380
[21] Li Y J, Wang B, Liu S R, et al. Fiber Bragg grating pulse and systolic blood pressure measurement system based on Mach–Zehnder interferometer[J]. Sensors, 2024, 24(19): 6222. doi: 10.3390/s24196222
[22] Jha R, Mishra P, Kumar S. Advancements in optical fiber-based wearable sensors for smart health monitoring[J]. Biosens Bioelectron, 2024, 254: 116232. doi: 10.1016/j.bios.2024.116232
[23] Guo J H, Zhang J Y, Dong L P, et al. Parallel waveguide fiber Bragg gratings–used for detecting human respiratory rate, trunk status, and pulse[J]. Opt Laser Technol, 2025, 181: 111960. doi: 10.1016/j.optlastec.2024.111960
[24] 李群, 陆云才, 邵剑, 等. 基于EpoCore胶裹覆的FBG传感器温度敏感性研究[J]. 光电工程, 2024, 51(12): 240228. doi: 10.12086/oee.2024.240228
Li Q, Lu Y C, Shao J, et al. Research on temperature sensitivity of FBG sensor based on EpoCore adhesive coated[J]. Opto-Electron Eng, 2024, 51(12): 240228. doi: 10.12086/oee.2024.240228
[25] 曾川, 童杏林, 李泽恺, 等. 基于线型光纤光栅阵列传感的引气管道泄漏研究[J/OL]. 激光技术, 1–16[2025-02-19]. http://kns.cnki.net/kcms/detail/51.1125.TN.20240423.2022.013.html.
Zeng C, Tong X L, Li Z K, et al. A research on the leakage of aircraft duct based on linear fiber grating array[J/OL]. Laser Technol, 1–16[2025-02-19]. http://kns.cnki.net/kcms/detail/51.1125.TN.20240423.2022.013.html.
[26] 何辰靖, 李志波, 赵强. 光纤布拉格光栅应变传感器应用综述[J/OL]. 光通信研究, 1–9[2025-02-19]. http://kns.cnki.net/kcms/detail/42.1266.TN.20241218.0826.002.html.
He C J, Li Z B, Zhao Q. Review of the application of fiber Bragg grating strain sensors[J/OL]. Opt Commun Res, 1–9[2025-02-19]. http://kns.cnki.net/kcms/detail/42.1266.TN.20241218.0826.002.html.
[27] Lin J H, Chen H, Ling Q, et al. Respiratory rate monitoring based on all-fiber strain-induced humidity sensor[J]. Opt Laser Technol, 2025, 181: 111840. doi: 10.1016/j.optlastec.2024.111840
-
访问统计


 E-mail Alert
E-mail Alert RSS
RSS
 下载:
下载: